Female hot flashes, a common experience during menopause, are not just a physical discomfort but also a complex interplay of hormonal changes, societal perceptions, and long-term health implications. This article delves into the causes, management, and impact of hot flashes, shedding light on this often-misunderstood aspect of women’s health.
From the hormonal rollercoaster that triggers these heat waves to the psychological toll they can take, we explore the multifaceted nature of female hot flashes, empowering women with knowledge and strategies to navigate this transition with confidence.
Causes of Hot Flashes
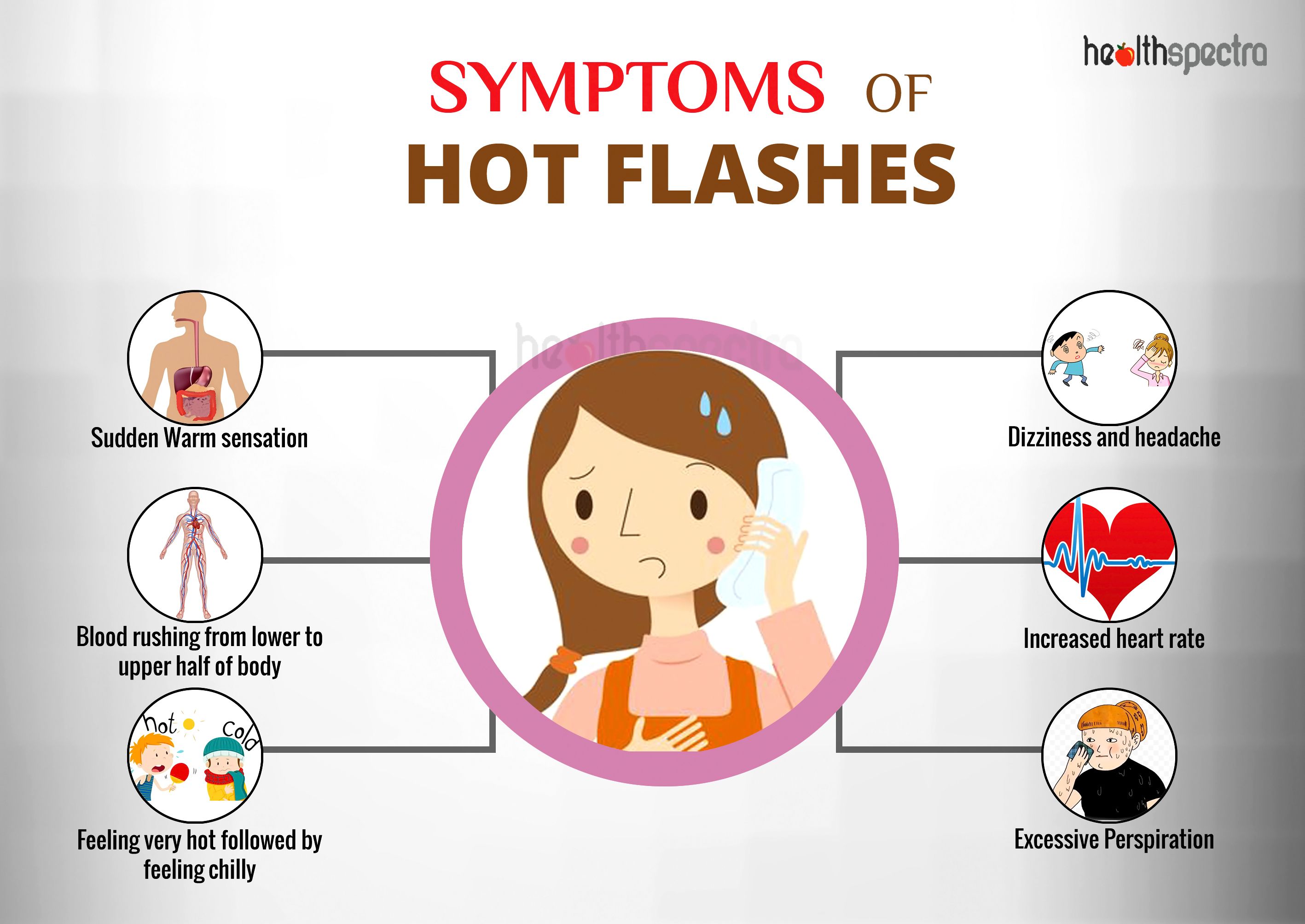
Hot flashes, also known as vasomotor symptoms, are a common experience for women during menopause. They are characterized by a sudden feeling of intense heat, often accompanied by sweating, flushing, and a rapid heart rate. Hot flashes can be disruptive and uncomfortable, and they can interfere with daily life.
The primary cause of hot flashes is the hormonal changes that occur during menopause. Estrogen and progesterone are two hormones that play a key role in regulating body temperature. During menopause, the levels of these hormones decline, which can lead to imbalances that trigger hot flashes.
Estrogen and Progesterone
Estrogen helps to regulate body temperature by widening blood vessels and increasing blood flow to the skin. This helps to dissipate heat and keep the body cool. Progesterone also plays a role in regulating body temperature, but its effects are less well understood.
When estrogen levels decline during menopause, the body’s ability to regulate temperature is impaired. This can lead to hot flashes, as the body attempts to cool itself down by widening blood vessels and increasing blood flow to the skin.
Obtain access to muscular strength training program to private resources that are additional.
Age and Menopause
The frequency and severity of hot flashes can vary depending on age and the stage of menopause. Hot flashes are most common in the years leading up to menopause and the first few years after menopause. As estrogen levels continue to decline, the frequency and severity of hot flashes typically decrease.
However, some women may continue to experience hot flashes for many years after menopause. This is more likely to occur in women who have a family history of hot flashes or who are overweight or obese.
Management of Hot Flashes
Managing hot flashes can involve a combination of lifestyle modifications, herbal remedies, and prescription medications. Understanding the triggers and potential remedies can help individuals find relief from these uncomfortable symptoms.
Obtain recommendations related to easy ways to stop snoring that can assist you today.
Lifestyle Modifications
Certain lifestyle changes can help reduce the frequency and severity of hot flashes:
- Maintain a healthy weight:Excess weight can contribute to hot flashes.
- Dress in layers:Wearing loose, breathable fabrics and layering clothing allows for easy adjustment during hot flashes.
- Avoid triggers:Identifying and avoiding triggers such as caffeine, alcohol, and spicy foods can help minimize hot flashes.
- Exercise regularly:Exercise can improve overall health and reduce stress levels, which may contribute to hot flashes.
- Stay hydrated:Drinking plenty of fluids helps regulate body temperature and reduce hot flashes.
Herbal Remedies and Supplements
Some herbal remedies and supplements may provide relief from hot flashes:
- Black cohosh:This herb has been traditionally used to treat menopausal symptoms, including hot flashes.
- Evening primrose oil:Rich in gamma-linolenic acid, this oil may help regulate hormone levels and reduce hot flashes.
- Soy isoflavones:These plant-based compounds have estrogen-like effects and may alleviate hot flashes.
Prescription Medications
In some cases, prescription medications may be necessary to manage hot flashes:
- Hormone therapy:Estrogen or progesterone replacement therapy can effectively reduce hot flashes.
- Selective serotonin reuptake inhibitors (SSRIs):These antidepressants have been shown to alleviate hot flashes.
- Clonidine:This medication, typically used to treat high blood pressure, can also reduce hot flashes.
Impact of Hot Flashes on Sleep and Quality of Life
Hot flashes can have a profound impact on sleep patterns and overall sleep quality. The sudden onset of heat and sweating can disrupt the sleep cycle, leading to frequent awakenings and difficulty falling back asleep. This sleep disruption can result in fatigue, irritability, and difficulty concentrating during the day.
Beyond sleep disturbances, hot flashes can also take a psychological and emotional toll on individuals. The unpredictable nature of hot flashes can cause anxiety and stress, leading to feelings of self-consciousness and embarrassment. The discomfort and disruption caused by hot flashes can also affect relationships and social interactions, as individuals may avoid situations where they fear experiencing a hot flash.
You also can investigate more thoroughly about 110v solar panel kits to enhance your awareness in the field of 110v solar panel kits.
Impact on Daily Activities
Hot flashes can significantly interfere with daily activities. The sudden onset of heat and sweating can make it difficult to concentrate and perform tasks effectively. This can lead to decreased productivity at work or school, as well as difficulty completing household chores or participating in social activities.
Long-Term Effects of Hot Flashes
Hot flashes, a common symptom of menopause, can have long-term health implications if not adequately managed. Research suggests that women experiencing frequent and severe hot flashes may be at an increased risk of developing certain chronic conditions.
Cardiovascular Disease
Studies have linked hot flashes to an increased risk of cardiovascular disease. The hormonal fluctuations associated with menopause can affect blood pressure and cholesterol levels, contributing to the development of heart disease and stroke. Women with a history of hot flashes have been found to have higher rates of coronary artery disease and peripheral artery disease.
Osteoporosis
Hot flashes have also been associated with an increased risk of osteoporosis, a condition that weakens bones and makes them more susceptible to fractures. Estrogen, a hormone that helps maintain bone density, declines during menopause. This decline can lead to a loss of bone mass and an increased risk of fractures, particularly in the hip, spine, and wrist.
Other Chronic Conditions
In addition to cardiovascular disease and osteoporosis, hot flashes have been linked to an increased risk of other chronic conditions, including:
- Type 2 diabetes
- Obesity
- Cognitive impairment
- Depression
Cultural and Societal Perspectives on Hot Flashes
Cultural and societal attitudes towards hot flashes vary widely across different regions of the world. In some cultures, hot flashes are seen as a natural part of aging and are not considered a medical condition. In other cultures, hot flashes are viewed as a sign of illness or weakness and may be associated with shame or embarrassment.
The impact of cultural beliefs and social norms on the experiences of individuals with hot flashes can be significant. In cultures where hot flashes are stigmatized, individuals may be less likely to seek medical help or to discuss their symptoms with others.
Discover the crucial elements that make best strength building workouts the top choice.
This can lead to feelings of isolation and distress.
Need for Increased Awareness and Understanding, Female hot flashes
There is a need for increased awareness and understanding of hot flashes as a normal part of aging. This can help to reduce the stigma associated with hot flashes and to improve the quality of life for individuals who experience them.
Conclusion
Female hot flashes are a reminder that the female body is a dynamic and ever-changing entity. Understanding the causes, management, and potential long-term effects of hot flashes is crucial for women to maintain their physical, emotional, and social well-being during this transformative stage of life.
By embracing a holistic approach that encompasses lifestyle modifications, medical interventions, and cultural sensitivity, we can empower women to reclaim control over their bodies and experience this transition with grace and resilience.
Clarifying Questions: Female Hot Flashes
What causes hot flashes?
Hot flashes are primarily caused by the decline in estrogen levels during menopause. Estrogen helps regulate body temperature, and its decrease disrupts the body’s ability to maintain a stable temperature, leading to sudden feelings of heat.
How can I manage hot flashes?
Lifestyle modifications such as staying hydrated, dressing in layers, and practicing relaxation techniques can help alleviate hot flashes. Herbal remedies like black cohosh and red clover may also provide some relief. In severe cases, prescription medications specifically designed to treat hot flashes may be considered.
Can hot flashes affect my sleep?
Yes, hot flashes can disrupt sleep patterns by causing night sweats and waking individuals up multiple times during the night. This can lead to fatigue, irritability, and impaired cognitive function.
Are there any long-term health risks associated with hot flashes?
Research suggests that women who experience frequent and severe hot flashes may have an increased risk of developing cardiovascular disease, osteoporosis, and other chronic conditions. However, more research is needed to establish a direct causal relationship.